BME faculty partner with UIUC to continue research into liver disease
block
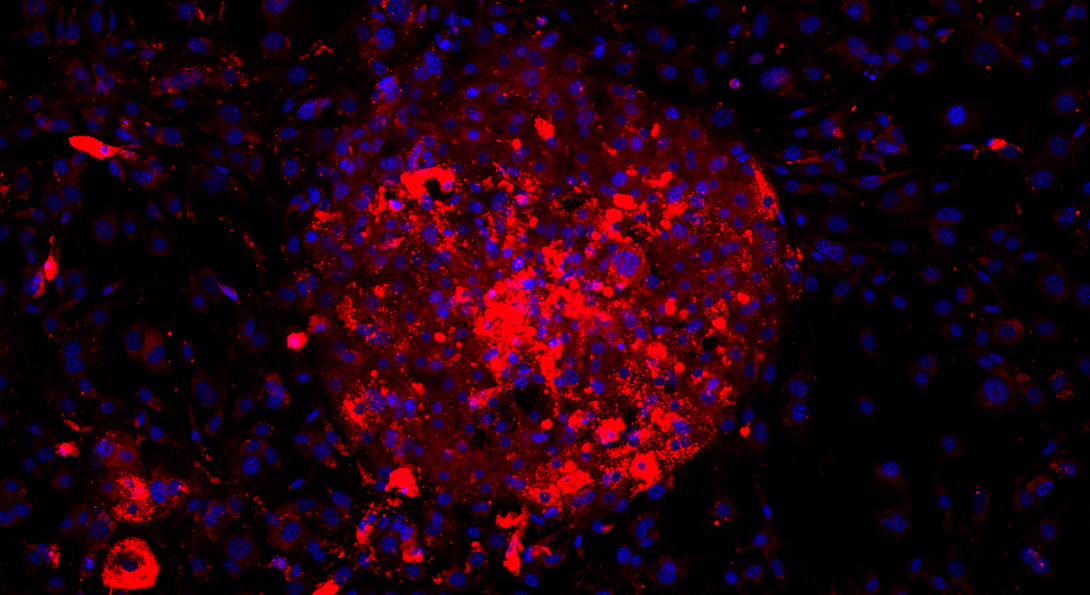
More than 2 in 5 adults in the U.S. have obesity (including severe obesity), according to the National Institute of Diabetes and Digestive and Kidney Diseases. In fact, obesity is an important risk factor for the onset of nonalcoholic fatty liver disease (NAFLD). Globally, nearly 70% of individuals with obesity have NAFLD. NAFLD encompasses many liver conditions that are characterized by excess accumulation of fat in the liver not related to significant alcohol intake and other causes of chronic liver disease. Often, NAFLD is associated with overnutrition and obesity.
As NAFLD progresses, the liver becomes fatty which can lead to scarring resulting in liver cancer and cirrhosis, among other effects. Because the liver is such a complex organ and does so many things for our bodies, the only treatment option currently available for patients is a liver transplant.
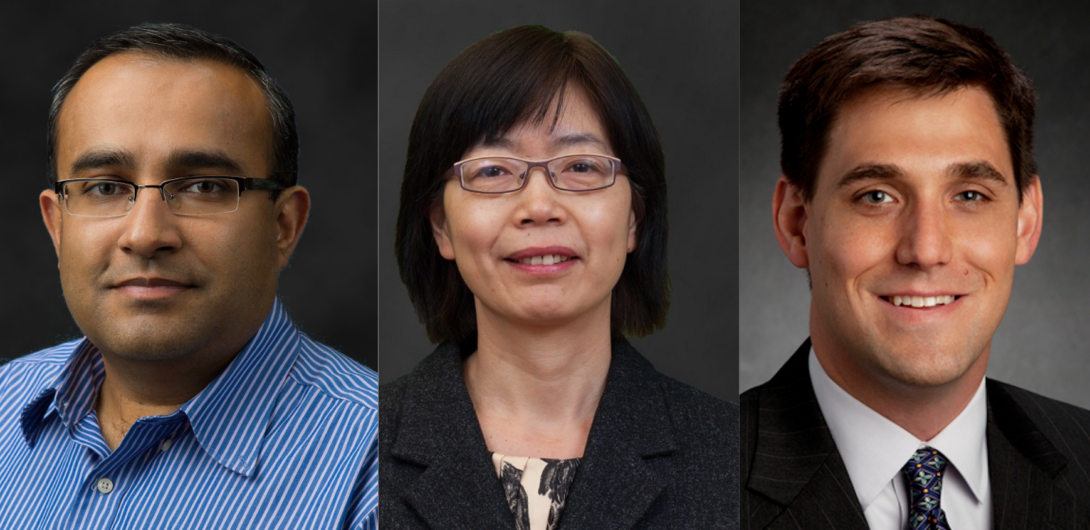
Richard and Loan Hill Department of Biomedical Engineering Professor Salman Khetani and University of Illinois Urbana Champaign Associate Professor Gregory Underhill initially received a NIH grant in February of 2018 and recently received a renewal to expand and continue their research. Khetani and Underhill have a long history of working together as trainees at Massachusetts Institute of Technology prior to Khetani joining UIC and Underhill joining UIUC as faculty members.
For the new grant, they recruited UIC BME Professor Yang Dai for her computational expertise. Their work will go through 2027, with the possibility of extending the project through 2028.
When Khetani and Underhill began their research, they focused on developing bioengineered liver models in vitro, which have significantly advanced our understanding of liver function and injury. They are useful for drug development and could ultimately lead to cell-based therapies. They hope ongoing development could lead to continual advances in bioengineered livers that show improving sensitivity for the prediction of clinically relevant drug and disease outcomes.
Khetani and Underhill have expanded their research to include four liver cell types rather than just two. The renewed research aims to better understand how specific cells can therapeutically be modified by medicines at a molecular and cellular level, which would improve disease models and aid the development of drug therapies. It will also help enable tools for a broad range of physiological and disease outcomes. Other researchers can then use the developed tools to create a cure for this silent disease.
Khetani and Underhill are also investigating epigenetics, the study of how our behaviors and environment can cause changes that affect the way our genes work. Epigenetic changes are reversible but can change how the body reads a DNA sequence. Their research will examine the role of epigenetic gene regulatory mechanisms and test the combined microenvironmental cues that regulate epigenetic changes, which are critical for the myofibroblastic programming of human liver cells within the context of normal and NASH triggers. Myofibroblastic cells persistent presence in tissues drives fibrosis, making them attractive cell targets for the development of therapeutic treatments.
“As you insult the body by causing damage, epigenetics change,” Khetani said.
The liver is made up of four different kinds of cells. Currently, strategies for targeting cellular modifiers of liver fibrosis remain limited because scientists are still working to unravel the mechanisms governing specific cell differentiation and the signaling between these liver cell types.
Dai’s contributions will include computational modeling of the epigenetic and transcriptomic data acquired from the fatty liver cultures to discover new pathways that can be treated with novel drugs in the future.
Khetani, Dai, and Underhill’s research uses living human cells rather than animal models. Animal models have long been used to get insights into NASH. However, despite researcher efforts, they don’t mimic humans exactly, and thus, not all human aspects are prevalent.
Khetani has been focused for much of his career on hoping to advance our understanding of this vital organ and advance our way to treat medical disorders, including NASH.
“I’m lucky to be working on a disease that matters,” Khetani said. “It’s a huge honor and privilege to be doing this research.”
Former students of UIC including, Chase Monkton, a 2022 graduate; David Kukla, a 2021 graduate; and UIUC graduates Aidan Brougham-Cook and Ishita Jain, both 2022 graduates, aided in this research. Owen Lally, a second-year doctoral student at UIC, and Nathan Shelton, a first-year doctoral student at UIC, will be contributing to the continuing research in collaboration with students in the Underhill lab.