Bioengineering professor receives NIH grant to develop a scalable 3D human liver platform for hepatitis B virus drug testing
Text block 1
Viruses that attack the human liver such as hepatitis B are some of the hardest to treat and study in part because of limitations with animal testing and traditional liver cell platforms. These problems have led researchers to look for new ways to screen drugs for diseases that impact the liver, with one of the most promising avenues of study being led by UIC Richard and Loan Hill Bioengineering Associate Professor Salman Khetani, who along with his lab and collaborators, has created scalable 3D human liver co-culture platforms.
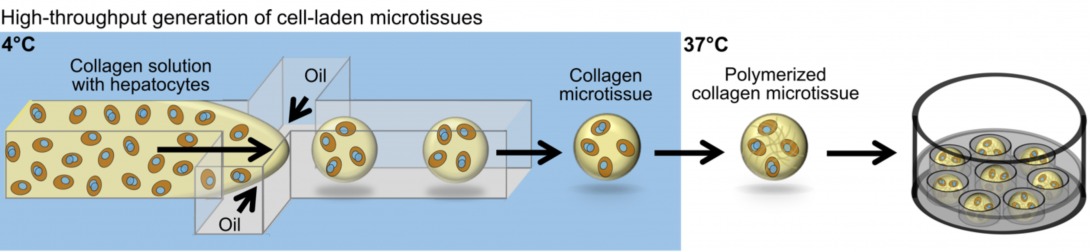
Khetani recently received a grant from the National Institutes of Health National Institute of Allergy and Infectious Diseases for $426,992 titled “A Scalable 3D Human Liver Co-culture Platform for Hepatitis B Virus Infection.” The money will help the researchers test the viability of infecting pioneered microscale 3D collagen microgels that contain induced pluripotent stem cell-derived human hepatocyte-like cells (iHeps) and other liver supportive cell types with HBV.
The work is critical, as around 240 million people are infected with HBV around the globe. Khetani said scientists have created vaccines to prevent initial infections, but once a person has the virus in their body it cannot be cured.
“You will be on drug therapy for the rest of your life because you have to keep the virus in check, so it does not overtake your liver,” Khetani said. “It’s a huge global burden. Pharmaceutical companies are really interested in developing drugs that are going to be curative.”
However, efforts to find curative drugs have been foiled by the tough preclinical testing environment surrounding the virus. Khetani said HBV is a human liver disease, so rodent models do not translate, and there are ethical and legal restrictions to testing HBV on non-human primates. He added the current in vitro human liver models on traditional plastic platforms lose their liver function after a few days and are unable to support HBV infection.
To get around these roadblocks, Khetani and his team used microfluidic devices to generate small 3D microgels, which they embed with liver cells. They then surround the microgels with a second cell type to complete the model. Initial experiments have shown these 3D liver models survive for weeks. The next step, which the grant will facilitate, is to see if they will support HBV infection for a longer period of time.
The grant will also allow the researchers to see if they can use induced pluripotent stem cells to support HBV infection in the model. This is important because these types of cells can be harvested from other cells in donors such as skin or blood, which means they are easy to find and gather, according to Khetani.
Additionally, the grant will help the team continue to improve their liver model to make it as close to the real organ in the human body as possible. Khetani said even though HBV only infects one type of liver cell, there are actually four different kinds of cells in a human liver involved in HBV disease progression, and the team plans to include all the key cells to get as accurate a model as possible.
“We are looking for that sweet spot with a sustainable cell source, the proper context in the liver for infection, a screenable format for this chronic infection. I think if we accomplish that we will have hit that transformative spot that is targeted to drug screening,” Khetani said. “If there was a magic bullet or drug out there (for HBV) it would have been discovered already. It’s going to be combination therapies and several generations of therapies and that all requires a robust screening pipeline.”
The 3D model could also be used to test drugs in other liver diseases such as alcoholic and non-alcoholic fatty liver disease. Khetani is also thinking bigger than just the liver with the model. He noted every organ has some dimension of 3D structure to it, so other cell types can be embedded inside the microgels. He has started working with some collaborators in the cardiology field to apply their techniques to cardiac muscle cells.
Khetani is collaborating with David Wood of the University of Minnesota and Jisu Li of Brown University on the HBV research. Yang Yuan, a UIC Bioengineering PhD student in Khetani’s Microfabricated Tissue Models Lab has also contributed to the project. Khetani added that his PhD student David Kukla developed this technology for the liver.
You can read more about Khetani’s lab here: http://mtm.uic.edu.